
General information
The tibialis posterior is one of the most central muscles in the leg. It is located within the posterior part of the leg. It acts as the key stabilising muscle within the lower leg.
Literal meaning
After, or behind, the shinbone.
Interesting information
Posterior tibial syndrome is a dysfunction of the muscle that results from flat feet or a fallen arch. There might be a history of injury to this muscle or it could be a first-time occurrence. Some confusion exists between this particular condition and that of tibialis posterior tendinopathy and the terms are used interchangeably. The meanings behind these two terms are different. A tibialis posterior tendinopathy injury is a painful injury to the tendon in the tibialis posterior.
Since the tibialis posterior muscle is responsible for the inversion of the foot, it will cause the arch to flatten when walking, standing or running when not properly working. In these instances, it can cause other injuries such as plantar fasciitis.
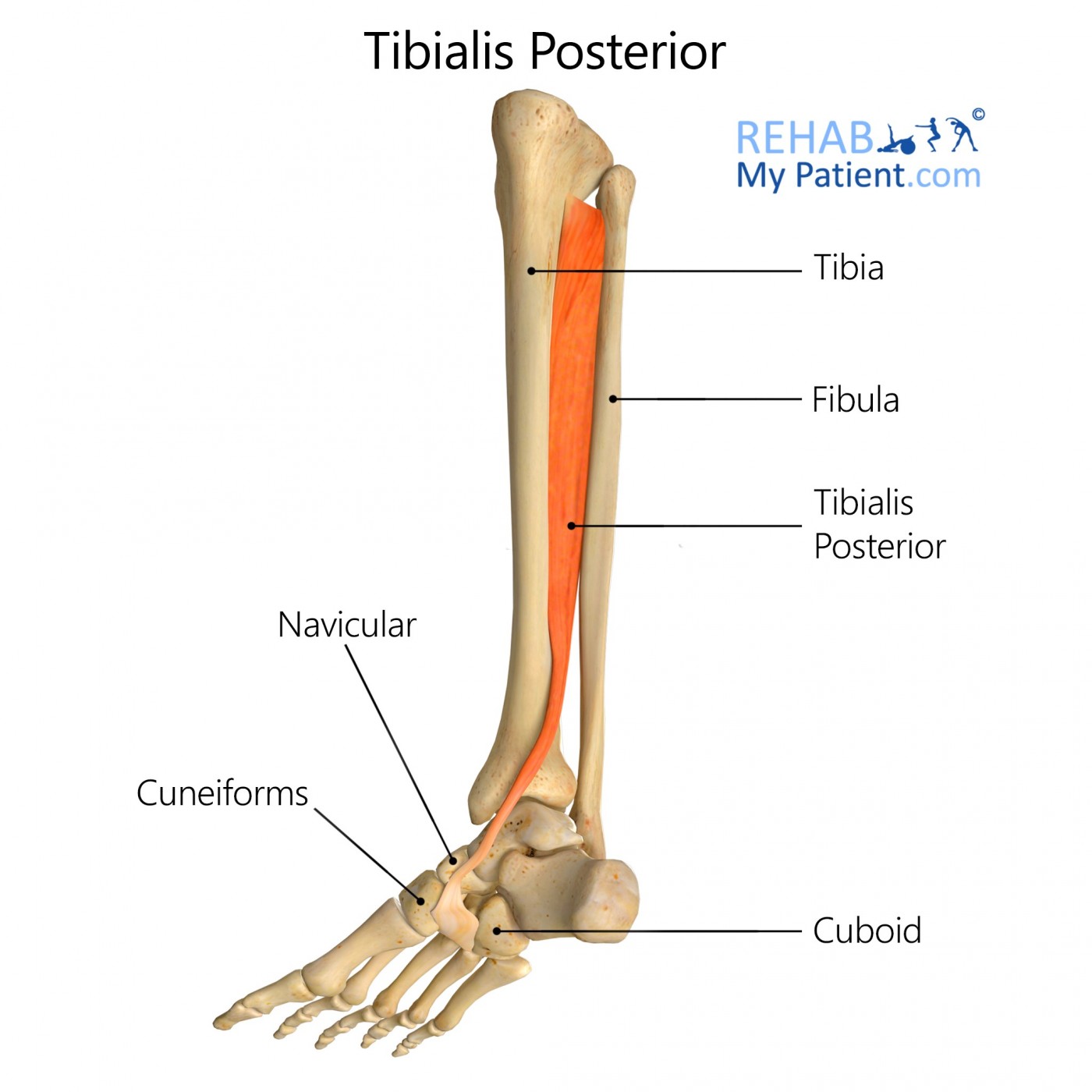
Origin
Posterior surface for the interosseous membrane as well as the adjacent surfaces for the fibula and tibia.
Insertion
Tuberosity for the navicular bone, plantar surface out of the medial cuneiform bone, tip out of the sustentaculum tali, plantar surface out of the intermediate cuneiform and the base of the second, third and fourth metatarsal bones.
Function
Primary inverter for the foot.
Aids in plantar flexion in the ankle joint.
Nerve supply
Tibial Nerve L4-L5.
Blood supply
Anterior tibial artery.
Posterior tibial artery.
Peroneal artery.
Medial malleolar artery.
Medial plantar artery.
Relevant research
Appropriate conservative treatment is imperative to addressing the symptoms associated with Tibialis Posterior Tendon Dysfunction (TPTD), and preventing long-term consequences. The main goal of the review, which was undertaken in 2007, was to evaluate the evidence from the various studies on the effects of conservative treatment modalities for managing TPTD. The aim was to use this information to help develop a clinical guideline for managing the condition. Studies were chosen based on a specific set of criteria and evaluated for quality. Preliminary searches identified no randomized controlled trials during the time of the review, so studies of lower hierarchy were also included. The review found five uncontrolled observational studies, but was not able to draw any conclusions from this about the best means of treating TPTD. The authors believe that further better quality research studies are required in order to reach a consensus on treatment for TPTD.
Bowring B, Chockalingam N. Conservative treatment of tibialis posterior tendon dysfunction--a review. Foot (Edinb). 2010;20(1):18-26. doi:10.1016/j.foot.2009.11.001.
Tibialis posterior exercises
Heel raises
For a beginner, it is best to perform this exercise while sitting in a chair. As it becomes easier, progress to some of the more difficult variations of the exercise. Raise the heels off the ground by pushing up on the balls of the feet. Pause momentarily and lower the heels back to the ground. Keep the toes on the ground throughout the exercise. Perform three sets of 10 reps. To increase the difficulty level, perform the exercise while standing. Start by raising both heels off the ground together and put them back down. If it becomes too easy, stand on a single foot at a time and use a table or chair for added balance.

Sign Up
Sign up for your free trial now!
Get started with Rehab My Patient today and revolutionize your exercise prescription process for effective rehabilitation.
Start Your 14-Day Free Trial