
Adhesive capsulitis tends to cause stiffness and pain in the shoulder. Over the course of time, the shoulder ends up becoming very hard to move. The condition only occurs in around 2 percent of the population. Most of the time, it affects individuals who are between 40 and 60 years of age. It occurs more often in women than it does in men.
The most common time to get adhesive capsulitis is following shoulder surgery, especially rotator cuff repair and shoulder decompression. This is probably due to the extent of arthritis in the shoulder that needed to be “cleaned-out”, which causes trauma to the shoulder. The resultant pain prevents mobility in the shoulder which then leads to stiffness. The stiffness gets worse and within two weeks the shoulder can be solidly frozen.
Other issues after surgery involve the use of a sling to protect the rotator cuff. A lack of mobility to the shoulder leaves the shoulder joint at risk of developing adhesive capsulitis (sometimes known as secondary stiffness).
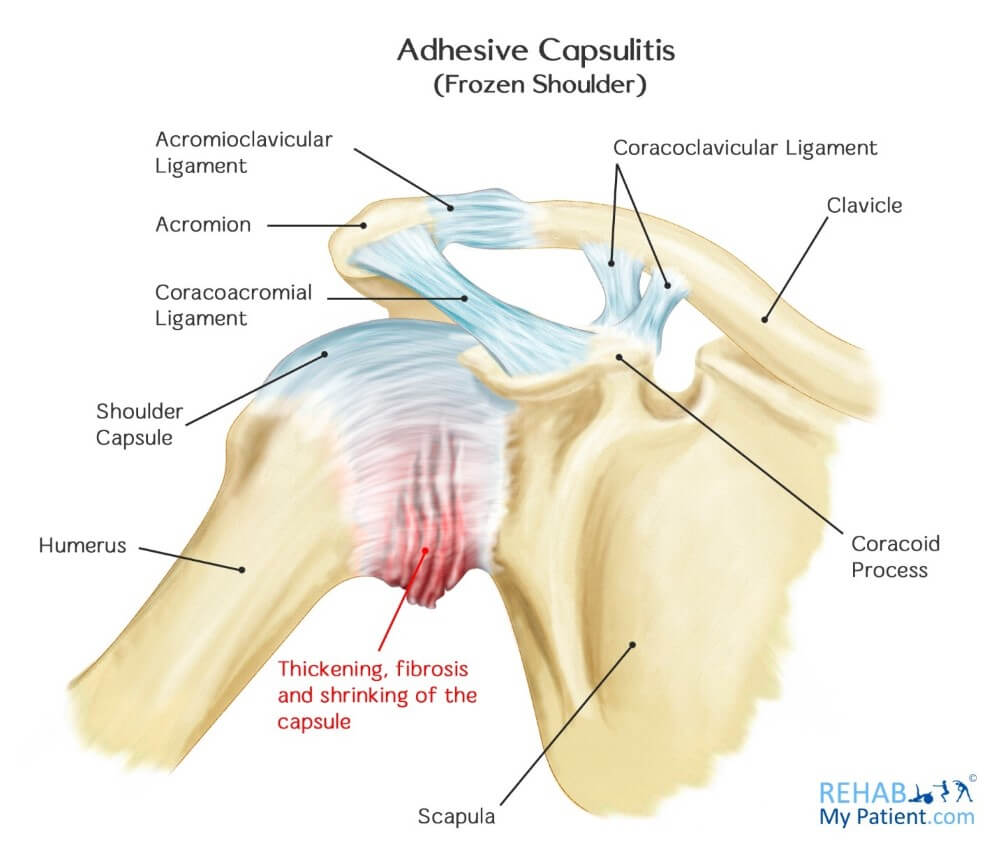
Adhesive Capsulitis Anatomy
The shoulder is a ball-and-socket type joint that is composed of three bones: the upper arm bone (humerus), the collarbone (clavicle) and the shoulder blade (scapula). The head of the upper part of the arm nestles into the shallow socket within the shoulder blade. Strong connecting tissues surround your joint. To allow the shoulder to move easily, synovial fluid serves as a lubricant for the joint and the shoulder capsule.
In terms of adhesive capsulitis, the capsule thickens and ends up tightening. Stiff tissue bands, known as adhesions, end up developing. In a number of cases, less synovial fluid is in the joint. One of the biggest signs of this condition is not being able to move your shoulder, regardless of whether that’s on your own or with the assistance of another individual.
Diagnosis is usually a combination of range-of-motion tests, performed first by the patient raising and lowering his or her arm, and then by the doctor manipulating the shoulder joint. An X-ray or MRI may be taken of the joint to confirm the diagnosis or to rule out any other disorders.
Adhesive capsulitis may develop in three stages (according to the text book – although just be aware this is not always the case). In the first stage, the “freezing stage”, patients usually experience pain associated with any type of shoulder movement, and their range of motion becomes limited. By the “frozen stage”, the pain may diminish, but the shoulder joint becomes stiff and the range of motion is significantly decreased. The third stage is known as the “thawing stage”, because shoulder mobility begins to improve. However, in a number of cases adhesive capsulitis will not improve without some kind of intervention (from physical therapy, or surgery) and the thawing stage never appears.
Cause
The cause of frozen shoulder is commonly unknown; however several risk factors have been identified. These include:
History of Shoulder Problems and Surgical Intervention
- Surgical - arthroscopy or rotator cuff repairs (most common cause) – known sometimes as secondary stiffness, the shoulder can seize up following rotator cuff repair. This is most often due to the arm being in a sling for 4-6 weeks, leaving the shoulder very stiff after the arm comes out. However, this can also be down to not doing the exercises after surgery. Sometimes frozen shoulder or secondary stiffness is unavoidable and due to the level of trauma experienced during the surgery to the bones.
- Trauma- fractures and dislocations. After dislocation, the shoulder can experience a lot of trauma and this causes the shoulder to form adhesions to protect itself.
- Previous conditions – a history of previous shoulder problems might increase your risk to getting frozen shoulder.
Other health Conditions can contribute to frozen shoulder:
- Diabetes
- Heart disease
- Stroke
- Lung disease
- Overactive thyroid (hyperthyroidism) or an underactive thyroid (hypothyroidism)
- Breast cancer
- Dupuytren's contracture
Age and Gender
Those most at risk are aged between 40 and 50. It has a higher prevalence in females compared to males.
How to Treat Adhesive Capsulitis:
- Anti-Inflammatory Medication Ibuprofen and aspirin can help to reduce swelling and pain. As the swelling decreases, the amount of pain that accompanies it will diminish as well. However many therapists discourage the use of anti-inflammatories because adhesive capsulitis takes a long time to resolve (often many months) and using anti-inflammatories for more than 2 weeks is not recommended.
- Steroid Injections Cortisone is a powerful form of an anti-inflammatory medication that can be injected directly into the shoulder joint. It can give patients a step-forwards but very rarely cures adhesive capsulitis.
- High Volume Injection Sometimes called hydrodilatation, a high volume of saline and steroid are injected into the shoulder capsule with the intension of stretch the capsule from the tight adhesions. The procedure takes about 15 minutes and is usually done under X-ray or ultrasound. Results vary but most people (around 70%) report some benefit from the injection.
- Physical Therapy Performing specific exercises can help to restore motion. This can be under the direct supervision of a trained therapist or performing them in the comfort of your own home. Therapy entails stretching and range of motion exercises for the shoulder joint. You can use a heat source or hot water bottle for loosening the shoulder before engaging in any stretching exercises. Therapists might also use other modalities including acupuncture, electrotherapy, ice and heat treatment and ultrasound.
- Surgery If your symptoms aren’t alleviated with therapy and using anti-inflammatory medication, you and your doctor can discuss surgery as an option. The most commonly used procedure is called an MUA (manipulation under anaesthesia). Essentially you will be under general anesthetic and the surgeon will move your arm firmly above your head and rotate your arm. Pops and clicks will come from the shoulder joint which mobilises the scar tissue. If the scar tissue is too thick, a capsular release may need to be performed where the capsule and scar tissue is cut by an electrical knife (during a keyhole procedure). The arm is mobilized at the same time to ensure full range of movement occurs.
More serious shoulder problems may require decompression surgery. It is important that you discuss the potential for recovery using simple treatments, as well as the risks associated with surgery. The goal of surgery for the condition is to stretch and release the joint capsule that is stiffened.
Tips:
- Adhesive capsulitis tends to occur more often in those who have diabetes, affecting around 10 to 20 percent of individuals. The reason isn’t known at this time.
- Adhesive capsulitis often develops following a shoulder surgery that has left the joint immobilized due to the surgery, fracture or other type of injury.
- Moving your shoulder soon after your surgery is one of the best methods for preventing adhesive capsulitis.
- Pain is often aching or dull. During the early part of the disease, the pain tends to be worse when you are able to move your arm. It is located over the outer part of the shoulder and into the upper arm.
- Follow the exercise rehab plan from your therapist. Failure to do regular exercises will significantly slow your recovery.

Sign Up
Sign up for your free trial now!
Get started with Rehab My Patient today and revolutionize your exercise prescription process for effective rehabilitation.
Start Your 14-Day Free Trial